Shoulder arthritis symptoms

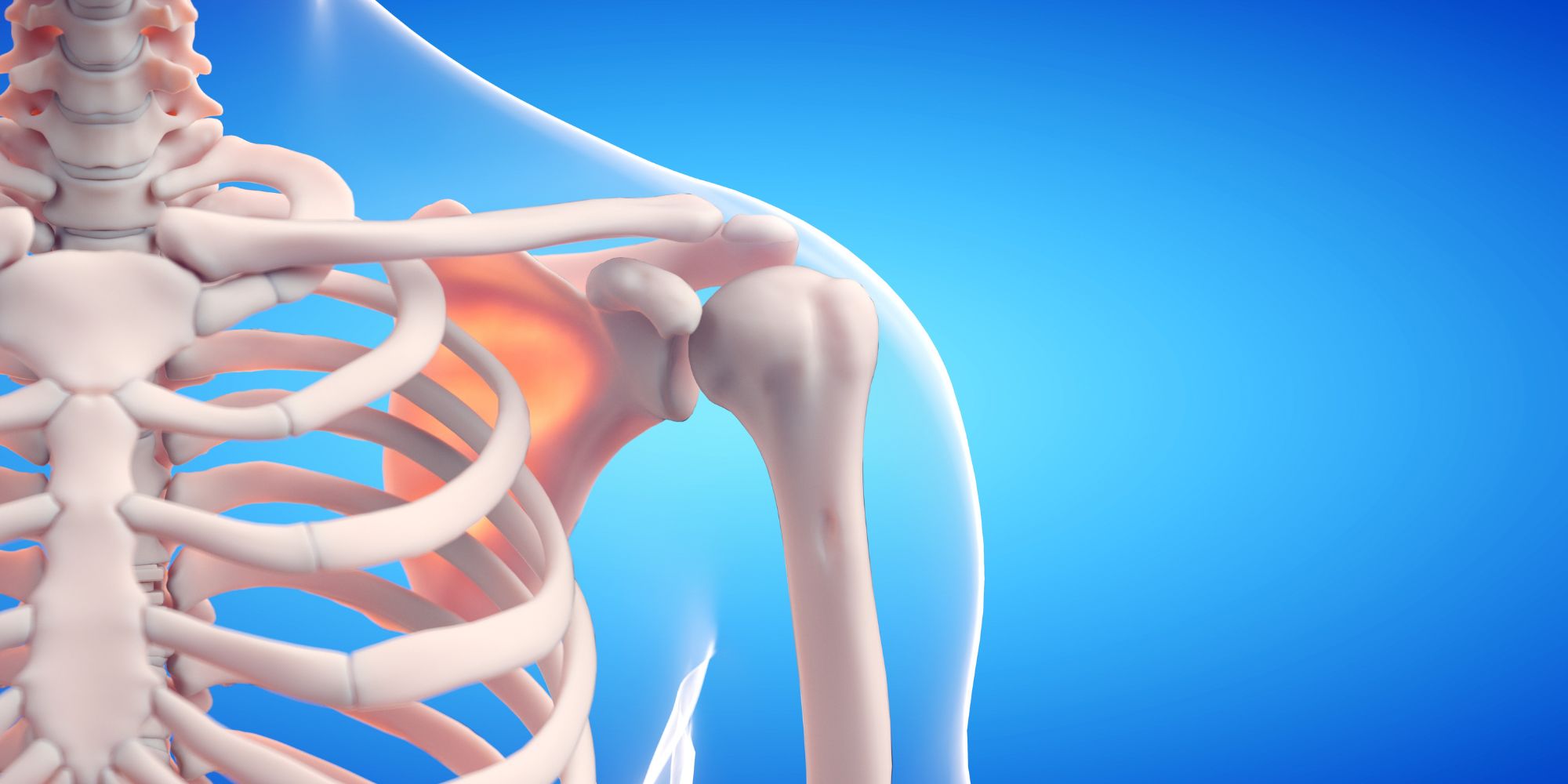
What is shoulder arthritis?
Shoulder arthritis is a degenerative joint disease that affects the shoulder joint. The shoulder joint is a ball-and-socket joint, where the head of the upper arm bone (humerus) fits into a shallow socket in the shoulder blade (scapula). The joint is covered by a layer of smooth cartilage that allows for smooth and pain-free movement. However, in cases of shoulder arthritis, this cartilage gradually wears away, causing the bones to rub against each other, resulting in pain, inflammation, and limited mobility.
Causes and risk factors of shoulder arthritis
There are several factors that can contribute to the development of shoulder arthritis. One of the primary causes is age-related wear and tear. As we age, the cartilage in our joints naturally begins to deteriorate, making them more susceptible to arthritis. Other risk factors include previous shoulder injuries, such as fractures or dislocations, repetitive shoulder movements, obesity, and family history of arthritis. It is important to be aware of these risk factors, as they can increase your chances of developing shoulder arthritis
Types of shoulder arthritis
The most common forms of arthritis affecting the shoulder include osteoarthritis, inflammatory arthritis, rotator cuff tear arthropathy, osteonecrosis, and post-traumatic arthritis.
- Osteoarthritis: Often referred to as a “wear and tear” arthritis, similar to that found in the hip and knee, it typically arises from a mix of factors such as usage, genetics, minor injuries, and increased stress on the joint. The cartilage deteriorates chemically, becomes rough and thin, and ultimately vanishes, leading to bone-on-bone contact that causes pain.
- Inflammatory arthritis: Seen in conditions like Rheumatoid Arthritis, various factors, often related to the immune system, trigger joint inflammation and lining damage, which erodes the cartilage surfaces. However, significant progress in the medical management of many inflammatory arthritis types has substantially reduced the necessity for surgical interventions.
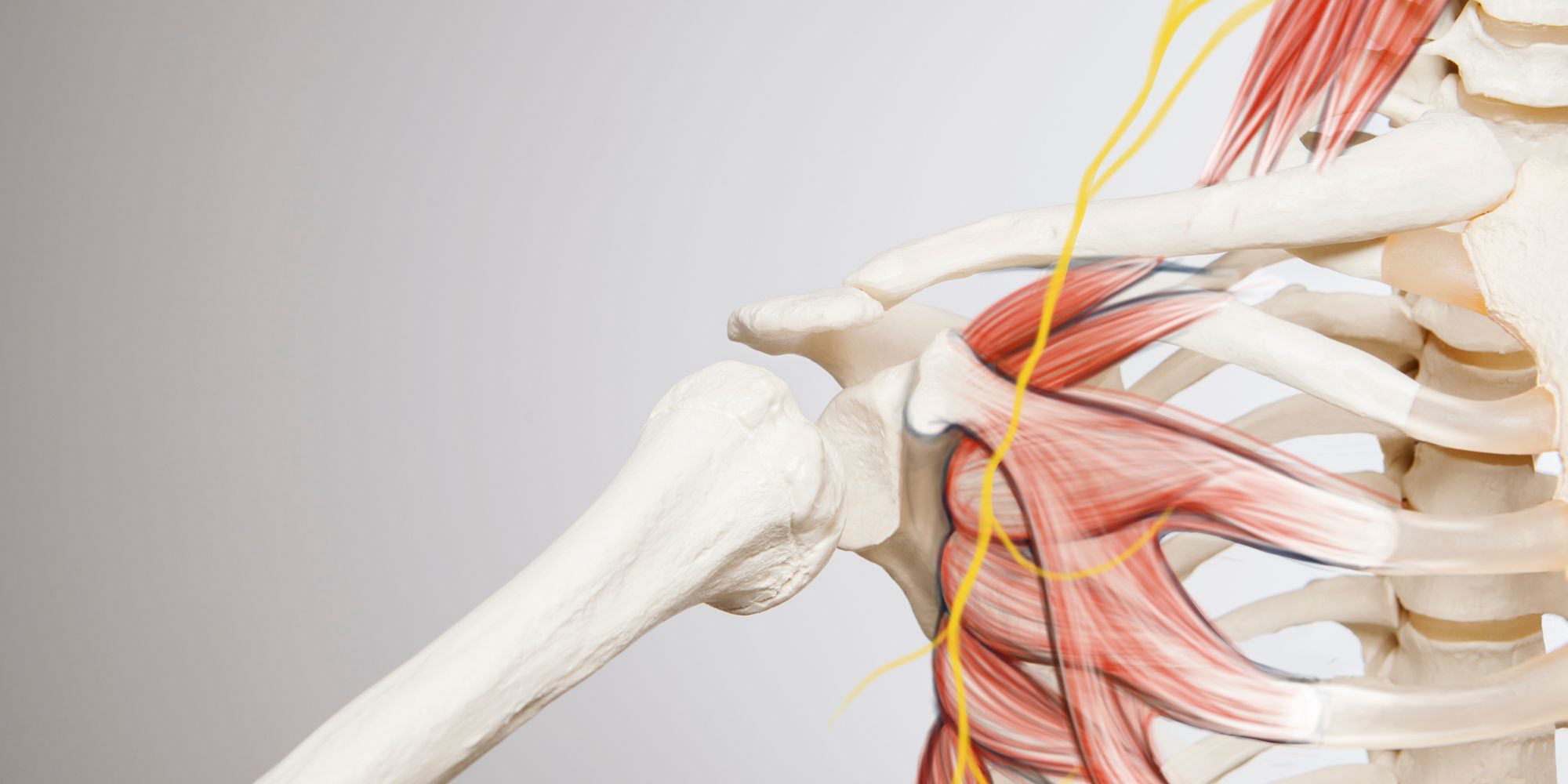
- Rotator cuff tear arthropathy: This condition represents the final stage of large, untreated rotator cuff tendon tears. It involves the dysfunction of the four key muscles that stabilize and move the shoulder joint. While large rotator cuff tears are rare, around 4% of patients with untreated tears develop cuff tear arthropathy. Managing shoulder arthritis from cuff tear arthropathy is challenging due to the combined damage to the joint’s soft tissue support and surface.
- Osteonecrosis: This rare condition occurs when the blood supply to the bone that forms the ball part of the shoulder is cut off, leading to the death and eventual collapse of a bone segment. As the bone support diminishes, the cartilage on top is subjected to increased stress, causing damage to the cartilage as well.
- Post-Traumatic Arthritis: This type of arthritis often follows a fracture of either the ball or the socket of the shoulder, where the cartilage is initially damaged along with the bone. Over time, this initial injury may lead to the cartilage wearing down and eventually deteriorating completely.
Common signs and symptoms of shoulder arthritis
Shoulder arthritis can manifest through various signs and symptoms. The most common symptom is pain, which is often felt deep within the shoulder joint and can be sharp or dull. The pain may worsen with movement or during periods of increased activity. Another common symptom is stiffness, especially in the morning or after prolonged periods of inactivity. You may also experience a decreased range of motion in the shoulder joint, making it difficult to perform simple tasks such as reaching overhead or behind your back. Swelling and tenderness around the joint, as well as a clicking or grinding sensation during movement, are also signs to watch out for.
Diagnosis of shoulder arthritis
If you are experiencing symptoms that may indicate shoulder arthritis, it is important to consult your doctor. Your doctor will start by doing a thorough physical exam and asking about your symptoms and medical history. They may also order imaging tests, such as X-rays or MRIs, to evaluate the condition of the shoulder joint and rule out other possible causes of your symptoms. Once the diagnosis of shoulder arthritis is confirmed, appropriate treatment options can be explored.
Treatment options for shoulder arthritis
Shoulder arthritis treatment aims to relieve pain, improve joint function and improve your quality of life. The right treatment option for you will depend on the severity of your symptoms, the type of shoulder arthritis and your overall health. Nonsurgical management options include medications to relieve pain and reduce inflammation, physical therapy to strengthen the muscles around the shoulder joint, and the use of steroid or hyaluronic acid injections. In more severe cases, surgical procedures, such as shoulder replacement may be needed. The doctor will guide you in choosing the most appropriate treatment option for your specific situation.
Non-surgical management of shoulder arthritis
Non-surgical management of shoulder arthritis focuses on relieving pain and improving joint function through conservative measures. Physical therapy plays a crucial role in strengthening the muscles around the shoulder joint and improving flexibility. Your physical therapist may recommend exercises that target the specific muscles involved in shoulder movement. In addition to physical therapy, pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed to alleviate pain and reduce inflammation.
Corticosteroid injections may also be administered to provide temporary relief. Because of the lack of evidence supporting their efficacy, however, no more than three corticosteroid injections in a single joint are recommendable unless there are special circumstances.
Some evidence exists supporting viscosupplementation for shoulder OA. In one study it has been reported that glenohumeral viscosupplementation resulted in a significant improvement in shoulder pain and function outcome scores 6 months following injection.
Lifestyle modifications, such as maintaining a healthy weight and avoiding activities that aggravate the shoulder joint, can also help in managing shoulder arthritis.
Surgical options for shoulder arthritis
Surgery is considered when pain persists despite nonsurgical options, with improved function being a secondary goal. The choice of surgery depends on patient factors like age, activity level, and disease factors such as lesion size and chondral involvement.
- Arthroscopic Treatment: Arthroscopy is a minimally invasive option for managing shoulder OA. It can serve as both diagnostic and therapeutic, providing relief for mild OA by stabilizing cartilage lesions and removing mechanical symptoms.
- Arthroplasty Options:
- Humeral Head Resurfacing Arthroplasty: This method involves placing a metal-alloy cap over the humeral head. It offers advantages like decreased bone resection and potential for revision surgeries if needed.
- Hemiarthroplasty: While providing short- to mid-term benefits, it may lead to glenoid issues and the need for total shoulder arthroplasty in the long term.
- Anatomic Total Shoulder Arthroplasty: This is considered the gold standard for advanced shoulder OA and often provides better outcomes compared to hemiarthroplasty. However, long-term concerns include glenoid loosening.
- Reverse Total Shoulder Arthroplasty: Recommended for cases with an intact rotator cuff, particularly when associated with massive rotator cuff ruptures. This method reestablishes the joint’s function by changing the joint’s center of rotation, providing good functional results.
Each surgical option has its pros and cons, depending on the patient’s condition and goals for treatment. It’s crucial to assess all available options in consultation with healthcare providers to determine the best approach for individual cases.
Lifestyle modifications for managing shoulder arthritis
In addition to medical interventions, making certain lifestyle modifications can greatly contribute to managing shoulder arthritis. Maintaining a healthy weight is crucial, as excess weight puts additional stress on the shoulder joint, exacerbating symptoms. Engaging in regular low-impact exercises, such as swimming or cycling, can help in maintaining joint flexibility and strengthening the muscles around the shoulder joint. Avoiding repetitive movements or activities that strain the shoulder joint can also minimize symptoms. It is important to listen to your body and avoid overexertion, as this can worsen the condition. Additionally, applying heat or cold packs to the affected shoulder and practicing relaxation techniques, such as deep breathing or meditation, may provide temporary relief from pain and discomfort.
Inclusion
Understanding the signs and symptoms of shoulder arthritis is essential for early diagnosis and effective management of the condition. By recognizing common symptoms, you can seek appropriate medical care and explore the various treatment options available, including non-surgical and surgical interventions, as well as lifestyle modifications. Remember to consult your doctor for an accurate diagnosis and personalized treatment plan. With the right approach, you can effectively manage your shoulder arthritis symptoms and improve your quality of life. Don’t let shoulder arthritis limit your mobility and enjoyment – take action today!
